Special thanks to the many influences that have contributed, directly or indirectly, to my questions leading into this #HITsm chat: @leonardkish @ochotex @avantgame @gzicherm @connected_book @paullikeme @robertamines @kellymcgonigal @joepine @hankgreen
Intro
I’ll be moderating the #HITsm chat on August 28th at 10am MDT and wanted to put together a couple of thoughts related to the topic before going into the chat. Maybe you’ll find these useful. Also, feel free to join us if you are interested in the topic. The more the merrier! Toward that end, let’s have a discussion about what we, in #HealthIT can do to make sure that we’re meeting the needs of those who are our end-users.
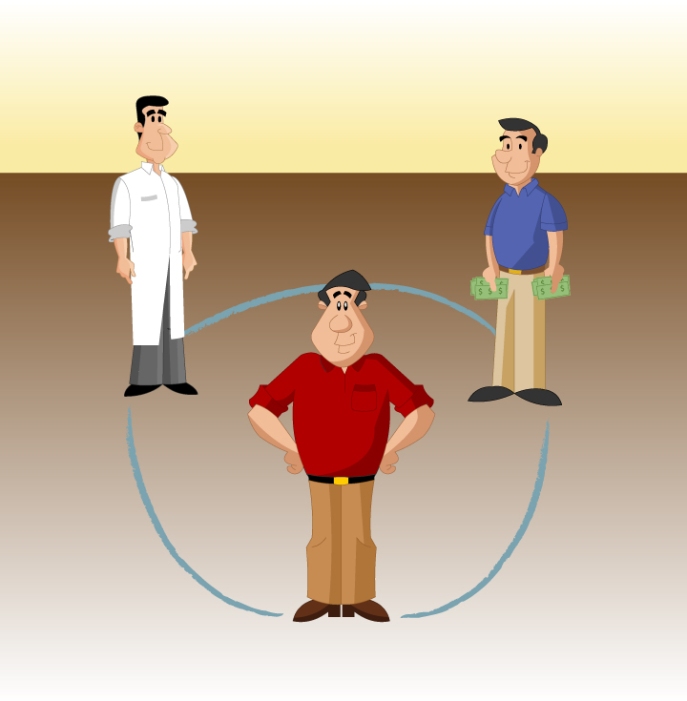
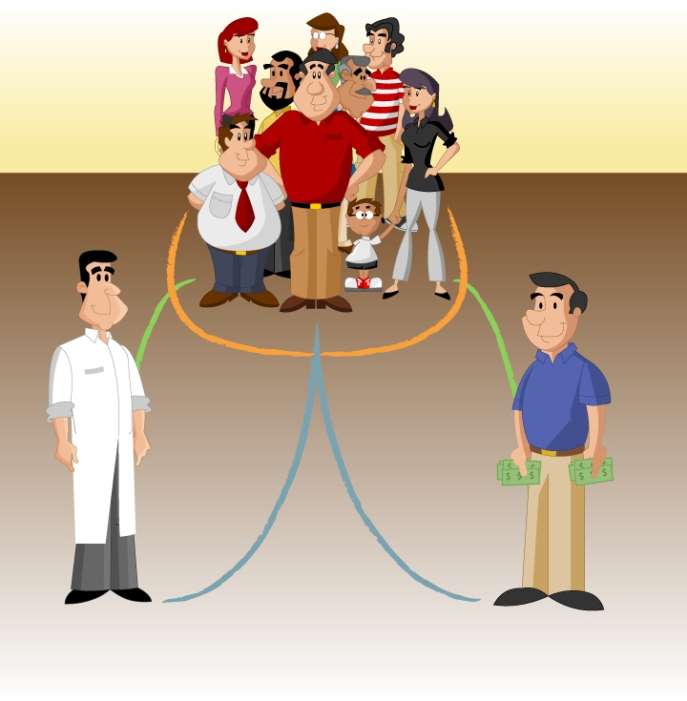
Considerations should include #EHR & #App design from #Payer, #Provider, #Patient, and #Peer per this posting on #4PHealth.
It’s the convergence of all four P’s (Provider, Payer, Patient, and that Patient’s Peers) that will allow for greater healthcare reach. When the Payer and the Provider are able to engage the Patient’s Peers, then true health generation is possible and the benefits of one’s social network can then be fully leveraged.
People:Person Design
We have historically looked at healthcare (and by extension, #HealthIT) as though it exists outside the “natural” world, or as though health is outside the realm of our social experience. Yet, we know that health is not divergent from our health reality or our everyday lives.
Healthy behavior is not dependent on what payment models, medical technology, or other innovations come about in the healthcare debate. We know that your friend’s friend has a great impact on what you do – and vice versa.
How do we reconverge these two realities knowing that what we do in our daily lives result in healthcare outcomes? Framed differently, how do we leverage the way we make decisions every day in considering how #HealthIT is designed?
Our health is not our own. We are bound to others, near and far, and by each decision and every sharing of those decisions, we birth our health.
#HITsm T1: Knowing that #health is dependent on daily life, how do we design #HealthIT in consideration of the larger, social world?
Cognitive Bias, Iterative Decision-making, Behavioral Economics, Game-Theory
Considering the depth of our knowledge related to cognitive bias, are we considerate of this branch of psychology in design? Knowing what we know about iterative decision-making (that decisions have to be made in sequence, often after new or different information) how do we prepare adaptive #HealthIT that responds to new information as it becomes available, like it does for Human Beings? For details on Cognitive Bias and Decision-making, see here and here. For Game Theory (including iterative decision-making), see here.
So what does a salutogenic framework look like? Mindfulness, resilience, focus on daily health-promoting activities that increase our ability to get healthier, rather than fend off illness. Of course, a fee-for-service model doesn’t bode well with this concept, so unless you’re enrolled in a highly visionary health promotion healthcare system, you’re probably on your own – for now.
Antonovsky’s explanation of Salutogenesis was well depicted by a river. His concern with the current model of health (Pathogenesis) is that it’s generally believed that we are healthy from the beginning but that because of environmental / circumstantial events, we become sick. Antonovsky expressed this as a river, where all healthy people stand on the bank, safe from the raging river’s flow. Once one stepped into the river – got sick – then something needed to be done. Salutogenesis, however, sees all people already in the river; but at different distances from the mouth.
There are some obvious benefits to these advances in Health IT, but one of the things that may not be fully clear yet is the application of Watson to understanding more about human behavior. While Watson can absolutely tell a clinician the likelihood of a set of symptoms’ association with a given disease, I’ll bet Watson can’t tell you how the patients’ family impacts their overall wellbeing through behavior reinforcement. If Watson knew who the patients’ workout buddy was, Watson might be able to help identify with a high confidence whether that workout buddy was a statistically-sound partner in the overall health management of the patient. Further, Watson would be able to weigh in on the evaluation of treatment adherence based on real-time data pouring into the health record for the given individual. This is the game state evaluation of the health of the individual in a real and meaningful way. With this, a total and complete understanding of the long-term treatment of chronic conditions (and even more important to the salutogenic framework that I’ve discussed previously in this blog series, total health production) through the understanding of actual human behavior devoid of the clinical separation from reality is the “social human” version of epigenetics that will become more useful in the coming years. This is where the data comes to life.
#HITsm T2: How do we achieve #patientengagement over time considering that a one-off solution can’t fix #health?
Gamification
A recent post mentioned that Gamification is failing due to a lack of accurately applying the concepts of gamification; in short, supplanting “badges” for increasing levels of difficulty appropriately. If Gamification is going to solve the #engagement problem, why can’t we quite figure this out? Gamification in health, generally, see here.
Whether we admit it or not, it is the promise of the potential emotional pay-off that lures us into working ridiculous hours already. But unlike gaming environments where we are totally immersed, our modern work environments seem contorted — almost criminally — to keep us from feeling blissfully productive. And once we give up hope that epic wins are possible, our careers turn into drudgery.
It takes more than a website to do this – including focus on using the resources available to a company’s natural habitat, the worksite, to engage employees during the 40 hour work week, and more, by creating a story. As described in the burgeoning world of Alternate Reality Games and Transmedia Storytelling, the ability to tell a cooperative narrative – on and offline – among those with which you work is an opportunity to actively create health, the benchmark of Salutogenesis. When you have many platforms for engaging in this storytelling, you increase the modes of access to actively engage all employees where they are, rather than forcing them into a platform that they may not be comfortable with, or is not ideal for their way of engaging in their health generating behaviors.
#HITsm T3: What game mechanics in #HealthIT are currently being used appropriately? Which are not?
Integration with the larger #healthIT world
Specifically looking at the #payer and #provider perspective, how can we ensure that the same #psych principles are being used to ensure adoption of #HealthIT throughout the Healthcare continuum? When we consider #wearables and #IoT, what do we focus on in terms of integration versus simple cataloging?
#HITsm T4: What should be made usable by #enterprise #healthIT to ensure the #Human element does not get lost?
Free-for-all on Design
#HITsm T5: What design considerations have you seen that work well in #HealthIT / #mHealth?
In review:
#HITsm T1: Knowing that #health is dependent on daily life, how do we design #HealthIT in consideration of the larger, social world?
#HITsm T2: How do we achieve #patientengagement over time considering that a one-off solution can’t fix #health?
#HITsm T3: What game mechanics in #HealthIT are currently being used appropriately? Which are not?
#HITsm T4: What should be made usable by #enterprise #healthIT to ensure the #Human element does not get lost?
#HITsm T5: What design considerations have you seen that work well in #HealthIT / #mHealth?
To our health,
Ryan Lucas
Manager, Engagement & Development